Show benign moles on the body. What are moles
Moles on the human body are a natural phenomenon.
You should not be afraid of their appearance, but you need to constantly and closely monitor the development of nevi.
This requirement is due to the fact that there are good and bad moles that can cause negative consequences.
- All information on the site is for informational purposes and is NOT a guide to action!
- Give you an ACCURATE DIAGNOSIS only DOCTOR!
- We kindly ask you DO NOT self-medicate, but book an appointment with a specialist!
- Health to you and your loved ones!
To distinguish between nevi that can harm your health, you need to know everything about the types of neoplasms and the signs of their degeneration.
This is especially true for those who have a lot of them.
Kinds
Moles are classified according to many distinctive features.
The most common distinction is the division of nevi into congenital and acquired.
More detailed classification - by size:
- small no more than 1.5 centimeters in diameter, there can be a lot of them on the body, face, limbs;
- medium - from 1.5 to 10 centimeters;
- large - more than 10 centimeters;
- giant - extensive in area.
According to the location, the following types of nevi are distinguished:
- epidermal, that is, arising in the surface layer of the skin - the epidermis;
- intradermal - formed in the dermis itself, in the depths of the skin;
- boundary - between the epidermis and dermis.
Each of these moles is a cluster of melanocytes, that is, pigment-containing cells.
They may not pose a danger, but may have signs and prerequisites for rebirth.
According to the internal structure, nevi can be vascular and non-vascular.

- Vascular are usually single and have a red, brown, bluish-brown color.
- There are several non-vascular moles at once.
When a lot of nevi are concentrated in one place, then the person begins to show anxiety. He is interested in the question, if there are many moles, is it good or bad? Doctors have only one answer to it: the main thing is that they are safe.
According to the form of neoplasms are divided into several subgroups:
- flat surface;
- lentigo;
- convex;
- blue;
- pigmented giant;
- dysplastic.

Reasons for rebirth
In order for good moles to be reborn, negative factors affecting them must be activated.
- A provocation of the dangerous development of nevi is ultraviolet rays.
- If there are a lot of moles, this is bad, because there is an additional risk of getting cancer. Usually, more than fifty nevi are considered dangerous; they can be on the face and other parts of the body. The total number of moles includes age spots and even freckles.
- Bathing in the sea in the heat also causes the rebirth of nevi. In this case, the effect of solar radiation through refraction in salt crystals is enhanced.
- Constant trauma to the nevus leads to its inflammation, and then to oncology.
- The influence of an unhealthy environmental background can also activate the change in a mole. Doctors say it provokes education cancer cells.
- Childhood and pregnancy are periods of active growth of moles due to a hormonal surge in the body. Women often think , if nevi appear, is it good or bad for the unborn baby? Safe nevi do not affect the health of the mother and fetus, and bad moles can harm the health of a woman, which can also affect the embryo.
- Finding nevi in traumatic places is very common cause the beginning of the transformation of the neoplasm. First of all, determine for yourself these areas in children, you will find photos of such areas on the Internet.
What is the difference between bad moles and good ones?

No one knows in advance what a mole that has appeared on the body will bring, whether its formation will have a good or bad effect on health.
How to distinguish a good mole and not panic?
Here are some expert tips on this:
- a good mole is not large;
- she has a clear outline;
- its tissue is homogeneous;
- the color scheme can be different from light to dark and even black shades, the main color should not change.
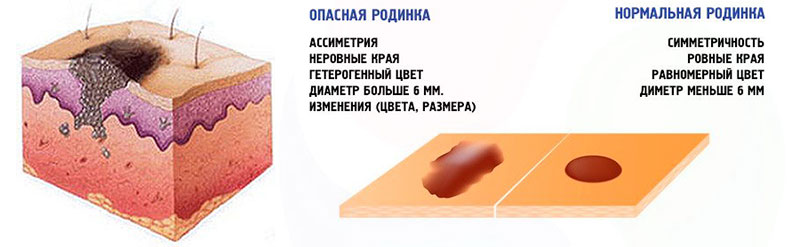
The combination of these principles is concentrated in the ABCDE rule (asymmetry + borders + color + diameter + transformation dynamics).
But only a doctor can make a conclusion about the benignity and malignancy of a mole.
Therefore, if the mole is black, it is not necessarily dangerous, black nevi are also good.
According to the ABCD formula, dangerous moles are also determined, with additional signs malignant mole are:
- mature age of appearance;
- change in color, size and shape;
- seals, expressions, peeling, bleeding on the body of the mole;
- the disappearance of the contours of the dermo pattern on the mole;
- the appearance of shine (gloss) or roughness on the surface of the nevus;
- wetting of the surface or a halo of hyperemia around the mole or nodules on it.
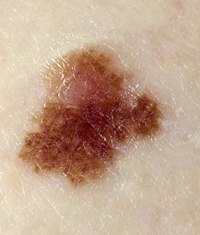
What does dangerous look like?
Based on the listed signs of the difference between good and dangerous moles, we can conclude about the appearance of the latter.
- They have changed color, shape and surface structure. A malignant mole has broken symmetry, one part is larger than the other.
- A dangerous nevus does not have a clear outline, the boundaries can blur.
- The color palette of a dangerous mole can be very diverse, absolutely different in tone, which is not typical for a benign nevus.
- The large size of the mole is also a bad sign.
- If the nevus smells bad and looks suspicious, then you should immediately show it to the doctor.
- If the hair growing in the nevus falls out, is it good or bad, there should be no question. This signal says that the mole is becoming dangerous.
When asked what to do when a mole smells, the doctor will answer that you should not self-medicate and eliminate the smell with flavors, perfumes, and so on.
It is necessary to immediately examine the nevus and determine the cause of the problem.
If moles look bad in older people, then the risk of melanoma, a malignant nevus, increases many times over.
This is facilitated by insufficient resistance of the body and flabbiness of the skin.
Knowing what signs dangerous moles have, it is possible to determine the beginning of their malignant degeneration in time, and to cure melanoma at an early stage.
If there are a lot of moles on the body, this is unlikely to end well.
Despite the assertion of fortune-tellers that the meaning of moles on a woman’s body often determines her happy fate, you need to monitor them and, if necessary, remove them.
A photo








Diagnostics
The main system for diagnosing moles is the result of an examination with digital equipment.
- The procedure is called epiluminescent video dermatoscopy. The device enlarges the nevus up to 200 times, which allows you to take a detailed photo of the tissues of the mole. Based on this examination, the state of the nevus is compared during the subsequent examination with the result of the previous one. This allows you to monitor the dynamics of its changes.
- The definition according to the ABCDE formula complements and refines the survey.
- In addition, a histological examination of dangerous moles is carried out. If the mole was removed, the histology of the material is done without fail. Next, doctors determine the course of treatment for the patient and decide what to do if the histology is positive. As a rule, additional examinations of the lungs, liver and other organs are prescribed. For example, a brain scan if the tumor is located on the head. Oral cavity and nearby organs are examined for melanoma on the lips, photos of such dangerous moles can be seen on the Internet.
Video: “Dangerous moles! Is it worth removing and how to recognize melanoma in time?
Signs of melanoma
Symptoms of melanoma are pronounced and hidden, signs are primary and secondary.
- Among the first signals are a change in the shape, size and color of the nevus, as well as unpleasant sensations in the area of the mole - itching, bleeding, roughness, burning, swelling of the surrounding area, the appearance of new pigments around the nevus.
- Secondary symptoms are more serious. This is the appearance of bleeding from a mole and pain.
- Metastasizing melanoma is characterized by the appearance of a cough, subcutaneous nodes and seals, enlarged lymph nodes, violations of the integrity of the skin in different places.
Treatment
Melanoma is treated in many ways.
- A malignant mole is surgically removed, its excision or deep removal of the tissues of the nevus itself and around it is done.
- A more gentle way is laser treatment.
It should be borne in mind that after removal, the wound heals slowly, especially for surgical intervention.
The hardware technology is characterized by a shorter recovery period and minor consequences of removal.
There are practically no traces on the body and face.
Chemotherapy and radiation are used to prevent recurrence of tumor development.
In order to choose a method of treatment, look at the reviews, how the removal ended and how many satisfied and healthy patients were after the operation. Such entries are in the journals of any clinic, as well as on the Internet. The price for operations in Moscow is affordable.
The cost of removing moles in prestigious clinics in Moscow
Prevention
To prevent the degeneration of a mole into a malignant one, it is necessary to monitor its development and consult a doctor if there are any signs of a change.
In addition, you need to protect yourself from sunburn, injuries, do not cauterize bleeding moles with iodine and use folk remedies only in consultation with the doctor.
Video: “Mole removal. Fast and painless"
Consider the types of moles and their meaning in order to understand the possible risks of formations on your body or their significance in your own destiny.
Marks on the human body can differ not only in size and color, but also in the nature of the occurrence, structure and danger to the health of its wearer.
Therefore, in modern medicine consider various types of moles, which are classified according to many parameters.
- All information on the site is for informational purposes and is NOT a guide to action!
- Give you an ACCURATE DIAGNOSIS only DOCTOR!
- We kindly ask you DO NOT self-medicate, but book an appointment with a specialist!
- Health to you and your loved ones!
Variety of nevi
Neoplasms on the skin may appear due to various reasons: pathological development skin cells before the birth of the child, fetal hypoxia, exposure to ultraviolet radiation, hereditary factor, individual characteristics leather, etc.
Therefore, it is possible to determine the diversity of nevi, based on the nature of their origin.
Consider various types of moles and photos describing the features of the neoplasm.
Vascular
Appear as a result of pathological transformation of blood vessels.
The color, size and bulge of such nevi depend on which vessel was deformed:
- if a capillary vessel began to grow, but a flat red spot becomes noticeable on the surface of the skin;
- when pathological changes begin to occur with veins and arteries, the vascular neoplasm will be convex, clearly visible and have a red or red-blue color.
Vascular moles can have a different manifestation, so there are two varieties of them: hemangioma and vascular malformation.
Hemangiomas
Such a formation on the skin is also called a strawberry spot because of its rich red color.
- They appear on the skin of babies in the first month of life: at first, light plaques are visible, then they gradually turn red and take on the appearance of swelling of the skin.
- Over time, its edges acquire clear boundaries, and the nevus itself becomes a bright red color.
- In this form, the nevus can be localized on the skin up to the age of seven children.
Acquired hemangiomas do not go away on their own, but can remain for life.
They have 4 varieties based on the nature of the appearance:
- arterial;
- venous;
- arteriovenous;
- capillary.
The most common sites of localization of such neoplasms are the neck and face.
Hemangiomas can not be removed if they do not cause aesthetic discomfort, because such nevi never degenerate into skin cancer.
Vascular malformation

It is another type of vascular moles, has a congenital origin and appears as a result of deformation of blood vessels.
Vascular malformation has two varieties:
- port wine stains can appear in children on the trunk, arms and face. From birth, the neoplasm has a light pink color, but soon they become bright or crimson red. During the crying of the child or when he rises heat, due to vasodilation, the color of the nevus becomes more intense. Port wine nevi remain for life;
- the bite of a stork appears on the body of a newborn as a result of great pressure on the skull of the fetus by the pelvic bones of the mother in the last weeks before childbirth. The spots have a reddish or deep orange color, irregular shape and fuzzy borders. The stork bite does not require treatment, it disappears on its own up to a year of the child's life.

Dark spots
Pigmented moles appear as a result of an excess in the skin cells of the coloring pigment - melanin.
- The amount of this substance directly determines the color of the neoplasm: from light beige and gray to brown and almost black.
- Nevi can have hairs and a different surface - smooth or rough, like warts.
They have 3 varieties:
Lentigo

This is the most common formation that is localized on the skin as a result of an increased accumulation of melanin in the tissues.
- Depending on its amount, the nevus can be from light brown to brown.
- Sometimes these spots look like freckles, but have a darker color.
- Lentigo on the skin can appear in old age as a result of the natural aging of the skin.
Mongolian spots

Such a formation looks like an accumulation of several bluish or brownish spots of irregular shape, it can form as a large continuous spot.
The place of localization is the lumbosacral zone.
Mongolian spots do not require treatment and go away on their own until adolescence.
coffee stains

Such nevi have a flat shape and the color of coffee with milk.
If no more than two such formations are found on the body, then there is no danger to health.
When there are more than two coffee stains, the patient is referred for examination to a neurologist, as this may be a manifestation of neurofibromatosis, a disease characterized by the appearance of a tumor from the cells of nerve endings.
White

If pigmented non-vascular neoplasms are the result of increased accumulation of melanin in skin cells, then white moles appear as a result of reduced production of melanocytes.
Such an outgrowth on the skin can be localized on any part of the body, have a different shape and surface structure.
- For the most part, neoplasms do not pose a threat to the health of their carrier and are a feature of the structure or transformation of the skin.
- But sometimes such moles are referred to as symptoms of a malfunction in some body systems, so they need to be shown regularly.
Video: “Mole removal. Fast and painless"
Types of moles on the body
Therefore, such moles were combined into separate group- melanoma dangerous nevi.
These include:
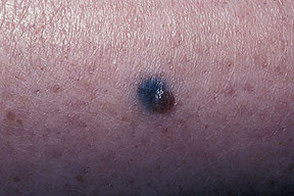
- blue nevus - the formation of blue or blue, may protrude above the surface of the skin. Hair on such a mole never grows. The size does not exceed 5 mm. Places of localization - buttocks, face and limbs;
- Dubreuil's melanosis is a pre-melanoma stage of skin formation. It is a single pigment spot of irregular shape and light brown color. Over time, the color becomes darker, the size gradually increases. On the initial stage diameter does not exceed 3 cm;
- A nevus of Ota is a large bluish pigment spot that can appear on a person's face. Education usually has light layers of skin and a heterogeneous structure;
- Setton's nevus - is represented by a red or brown nodule raised above the skin, the size of such a formation is up to 5 mm, oval in shape. A distinctive sign of such a nevus is a depigmented ring that surrounds the formation on all sides and has a larger diameter than the mole itself;
- pigmented border formation - a flat dark-colored nevus with a smooth surface on which hair never grows. The size of such moles is no more than 1 cm.
- giant pigmented neoplasm - a large nevus, the surface of which is heterogeneous: cracked, bumpy or warty. Such a mole increases as the person himself grows;
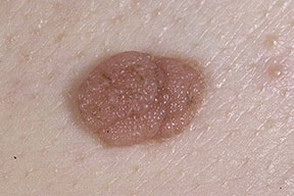
- papillomatous mole - a formation with irregular outlines and a heterogeneous surface. Size - up to 2 cm. They can match the skin in color, or they can have dark brown or grey colour. It is localized more often on the scalp, while hairs also grow from it;
- verrucous neoplasm - a variation of the previous type of nevus, but with a difference in surface structure: it is more pigmented and bumpy. The nevus itself has many deep cracks.
Photo of melanoma dangerous nevi








Signs of melanoma
In order to identify melanoma in the early stages, dermatology has developed a simple test for this called AKORD.
Let's decipher its essence:
- BUT- asymmetry of two equal halves, which are located on both sides of the visually drawn axis;
- To- the edge of the mole has denticles or bumps;
- O- the color of the formation is uneven, interspersed with a different color;
- R- the size of the nevus is constantly increasing;
- D- the dynamics of education: growth, discoloration, the appearance of cracks, crusts,.
If at least one point from the above test can be applied to any mole on your body, then this is a reason for an urgent visit to an oncodermatologist.

Meaning
According to astrologers, each mole has its own meaning, in a certain way influencing the fate of its carrier.
Therefore, consider what the nevi on the body and face of a person mean:
- a nevus on the face means the beauty and attractiveness of its owner. May indicate success in creativity or business. Education on the forehead will indicate the diligence of a person and the luck that accompanies him all his life. A nevus on the cheek is a sign of benevolence and security in life;
- a neoplasm on the neck is a good sign, but only if it is located in front;
- on the shoulders - a sign of wisdom and prudence. Such people show themselves to be good partners in life;
- a mole on the left hand will tell about a person who is very hardworking. Nevus on the right is a sign of a successful career;
- education on the chest speaks of the self-confidence of its owner. For a woman, such a sign means that she will become a good mother;
- nevus on the back - a sign of honesty and devotion, on the stomach - wealth;
- a mole on the legs is a sign of a large number of difficulties on the path of life.
Sometimes moles on the body form special signs that have a unique meaning:
- in the form of a triangle happy life its carrier. If the nevi are grouped in the form of a triangle on the arm, then such a person will be very rich. If three moles are located side by side on the face - a sign of success in creativity.
- the arrangement in the form of a star speaks of the exceptional talent of a person.
- in the form of a heart - a sign of great love in the life of its owner.
- nevi like constellations are a fateful sign and mean that a random event can change the course of one's usual life.
- when moles are arranged in the form of the constellation Ursa Major, then a person’s life is constantly filled with interesting events.
Having learned what this or that mark on your body means, you can discover new facets in yourself.
No matter how fateful the value of a mole may be for you, if you suspect its malignancy, you must definitely get rid of it.
Video: "The meaning of moles on the human body"
Most people have moles. For some, they appear from the first days of life, while someone first discovers them only in adolescence or even later. They give charm and charm, but are not as harmless as they seem. What moles are considered dangerous and how to identify them in time?
We take nevi under special control
In medical terminology, moles are called nevi. This is a benign structure that indicates a congenital defect in the development of the skin.
The only and main complication of a nevus is its transformation into a malignant formation. In the advanced stage, cancer cells enter the bloodstream and spread the cancer throughout the body.
The most aggressive tumors arise on the basis of the blue nevus, nevus of Ota and borderline nevi.
blue nevus
It occurs mainly in people with dark skin color, its carriers are people of Asian origin. It looks like a small smooth dense spot that protrudes slightly above the skin. The characteristic color is blue and all its shades. Neoplasm is prone to constant increase. At some point, growth can become rapid and uncontrollable - and this is already a sign of the development of melanoma - skin cancer.
Oncologists suggest removing blue nevi immediately after they are detected!
Nevus of Ota
Like the previous type, these dangerous moles are overwhelmingly found among Asian peoples, especially among the Mongols and Japanese. It is a gray-blue spot located on the face. Size - at least a few centimeters in diameter. May affect mucous membranes, sclera and cornea of the eye.
Its size, combined with an overabundance of the sun, is blamed for its transformation into a malignant form. Indeed, it is impossible to completely protect such a vast area from UV exposure, because the number of sunny days in Asian countries reaches 300 or more. For comparison, Moscow can only enjoy 70 sunny days a year.
Borderline nevi
Such pigment formations are called borderline, since they are localized on the border of the dermis and epidermis. This is a congenital mole that grows evenly with the growth of the whole organism. Its dimensions are insignificant - 2-3 mm. The color is usually dark, sometimes changing towards the periphery, forming concentric rings. Thickening or a significant elevation above the skin is the first sign of rebirth.
Risk group
Almost all people have pigmented and vascular formations on the skin, such as moles. However, some people are more likely than others to find dangerous moles in themselves. Why? It's all about the initial amount of melanin in our skin, in other words, skin color. The second reason is the presence of a large number of nevi on the body. The third reason is heredity.
Phototype
There are three main skin types. You can determine your type yourself by remembering how your skin reacts to sunburn:
- Phototype 1. Under the influence of sunlight, the skin turns red, but never tans. People with very fair skin, blond or red hair are prone to such reactions. Their frequent companions are freckles.
- Phototype 2. After insolation, the skin turns red, and then pigmentation appears - a tan. This type includes people with dark skin and blond hair, brown and (rarely) blue eyes.
- Phototype 3. Tan "taken" immediately, without redness.
Owners of phototype 1 - white-skinned, fair-haired and blue-eyed - should especially carefully monitor their skin. These people are at high risk!
Number of nevi
The very fact of having moles on the body is already a risk factor for melanoma. The more such marks, the higher the likelihood of developing the disease. This is especially true of the melanoma-dangerous types of nevi described above and the presence of a large number of convex formations.
hereditary factor
Most of the moles become dangerous due to the impact on them of provoking factors - sunburn and injuries. However, 1/3 of dangerous moles appear due to a genetic predisposition. So, if there were 2 cases of melanoma in the family history, then the probability of the disease in the offspring tends to 100%.
Signs of degeneration of a mole
People who are well aware of the danger that moles are fraught with react much faster to the slightest changes in their structure and go to the doctor more often. How to maintain your health and not miss the first signs of a terrible disease?
Self inspection. Learning ACORD.
This is the key point. You need to know all your moles "by sight". If any of them seems different from the rest and looks suspicious, this is already a reason to visit an oncodermatologist.
There is a simple formula that is easily applicable for self-diagnosis and determining which moles are dangerous. It is an abbreviation for AKORD.
- A is asymmetry.
- K - edges.
- Oh, coloring.
- R - size.
- D - dynamics.
So, a symmetrical mole with smooth edges, uniformly colored, not changing its size is considered harmless. In general, any change in the nevus should already be alarming. Dangerous and requiring immediate consultation with an oncologist, there will be such manifestations:
- Peeling.
- Bleeding.
- Change of size.
- Change in color, especially heterogeneity.
- The appearance of redness along the contour.
Timely diagnosis
To determine the good quality of a mole, the following non-traumatic, and therefore safe, methods are used:
- dermoscopy;
- computer diagnostics;
- laboratory diagnostics.
Dermoscopy uses a special device called a dermascope. With its help, the structure of the nevus is examined at high magnification. Unfortunately, not every state clinic has such a device.
Computer diagnostics - a photo of a spot is compared with spots from an extensive database. This facilitates and speeds up the diagnosis to the doctor. However, histological analysis within the framework of laboratory diagnostics gives results already at the cellular level. In this case, work is underway to identify tumor markers and gives the most accurate results.
In addition, the removal of a suspicious nevus is always followed by histological analysis. The result of such a microscopic examination is the determination of the presence or absence of oncogenicity and its degree.
Safe Life Algorithm
There are simple rules, following which we can significantly reduce the risk of a harmless mole turning into a melanoma-dangerous one.
We do not injure
If the nevus is located in places of constant friction, then the most correct action would be to contact a dermatologist and remove it.
Owners of a large number of moles should not use hard washcloths when taking a shower. Only sponge.
You can not remove a mole on your own, even if it "hangs by a thread." It may be dangerous!Don't get tanned
Excess ultraviolet radiation has a very negative effect on the health of our moles. It is not for nothing that since 2011 in California, children under 18 are prohibited from using tanning beds at the legislative level, even with the permission of their parents. This rule was introduced after many years of research, during which it was found that from the moment of tanning in a solarium to the development of melanoma, it takes from 5 to 25 years.
Identification of a dangerous mole in the early stages in most cases leads to a complete recovery. Keep track of your moles, take pictures of them and measure them with a ruler. Treat them carefully and reverently, and they will forever remain just a cute decoration that emphasizes your individuality.
Nevi on the body are otherwise called birthmarks, moles, and are benign formations that appear on the skin. Moles are either on the same level with the skin, or rise above it, the reasons for their appearance are varied, mainly a genetic predisposition and a certain type of skin. The sizes of the nevi shown in the photographs below vary from very small (1-2 mm) to large (15-25 cm).
Color, depending on the cells that formed it, can be:
- bodily;
- red;
- brown;
- purple;
- almost black.
Benign formations can occur not only on the skin, but also on the mucous membranes (for example, in the vagina), connective membranes, the edges of the lips, the vessels of the eye as a spot, a skin phenomenon consisting of nevoid cells.
Nevi are congenital and acquired. Educational cells appear even in the prenatal state of a developing human body. They originate in the neural crest, a "cell storage" that serves as the basis for the formation of various anatomical structures.
According to statistics, almost 80% of white-skinned representatives of the world's population have nevi on their bodies. In adults, the number can be 30 pieces or more. AT childhood they may not be, but during puberty, during pregnancy, under the influence of sun activity, nevi appear on the skin.
A benign formation, developing, goes through several phases:
- intraepithelial (initial);
- border;
- intradermal (at the age of 30 years);
- reverse (in old age, the cells “return” to the layers of the skin).
Nevuses are accumulated nevocytes containing a large amount of melanin. Nevocytes are called changed melanocytes - cells that determine the shade of human skin. When exposed to sunlight, melanin appears in them, giving the skin a tan color.
It's important to know ! The shapes and sizes of birthmarks are so diverse that they are confused with some dermatological pathologies: "skin horn" (fibroma), seborrheic keratosis, papillomas. Therefore, only a specialist is able to make an accurate diagnosis by differentiation. Often, this requires a histological analysis to study the taken tissue biomaterial.
Causes of the appearance of nevi
Impaired embryogenesis causes the development of congenital nevi. They may have hereditary traits and serve as proof of belonging to the same genus.
"Children's" melanocytic nevi appear under the following predisposing conditions:
- exposure to toxic compounds, radiation on a woman carrying a child;
- the presence in pregnant women of pathologies that have developed in the urogenital tract;
- toxicoses, threats of termination of pregnancy;
- hereditary unfavorable predisposition.
The following provoking factors contribute to the occurrence of acquired nevi:
- hormonal "explosion" in puberty;
- pregnancy period with hormonal fluctuations;
- taken oral contraceptives;
- skin pathologies of infectious and allergic nature;
- injury to the skin as a result of mechanical action;
- insolation (exposure to direct solar radiation);
- the impact on the human body of radiation, x-rays;
- diseases of viral etiology.
Types of nevi
The classification of nevi according to histological features gives an assessment characteristic features any type of formation, which contributes to an effective prognosis of the course of the disease. There are more than 50 types of birthmarks, of which ten nevi are common.
The conditionality of the division into groups concerns tumors:
- Melanoma dangerous (having a tendency to degenerate into malignant formations).
- Melanoma-hazardous (not having a tendency to degenerate into malignant formations).
Melanoma formations include the following types of nevi:
Blue
Such a single formation, which is an accumulation of melancites, is in a precancerous state, although it is called benign. At the same time, it has no tendency to oncological degeneration. The color of the nevus - bluish or blue-black - depends on the active production of melanin by the cells of the nevus. It has the correct shape, evenly outlined contours. Due to the elevation above the skin level, such a nevus can often be injured by details of clothing, jewelry, etc. Patients with such a birthmark should be regularly examined with preventive purpose to prevent rebirth into malignant tumor.
Border pigment
This is an innate formation that manifests its characteristics immediately in the first periods of a person's life. The nevus develops along with the growing organism, even without any external factor. A brown / brown / black spot can reach a diameter of 1.5 mm to two to three or more centimeters. Such nevi "settle" on the palms, feet. Malignancy can manifest itself after injury or prolonged exposure to the sun.
Nevus of Ota
The manifestation of the skin phenomenon is directly dependent on the nervous factor. A spot consisting of a large amount of melanin is localized on the most exposed part of the body - the face. Black and blue formation of a genetic orientation is found in representatives of the Asian race.
Melanoma dangerous nevi , in turn, there are several types:
Intradermal pigment
These moles, which form in the dermal layer, under the skin, are mainly recorded during adolescence. They are initially small in size, but grow and develop with the body of a teenager. Nevi of this type are practically not able to degenerate into malignant ones. Only under the influence of certain factors there is a risk of melanoma.
Such formations can be located on the neck, in the groin, armpits, under the mammary glands, sometimes on the upper and lower limbs, body skin.
Papillomatous
This type of nevus has a repulsive appearance being a cosmetic defect. A brown or pink mole in the form of a growth rises above the level of the skin, has a soft granular surface, and when palpated, it responds with soreness.
There are such moles on the head under the hair, they are also found on the body. The growth of formations is slow, the transformation into a malignant formation is practically not fixed.
Galonevus
This birthmark is also called Setton's nevus. It appears in people who have a weakened immune system due to hormonal failures, autoimmune pathologies.
Galonevus is characterized by an oval shape, large size, elevation on the skin. The formation is localized on the trunk, upper and lower extremities. There are both single and multiple nevi, but they do not degenerate into malignant tumors.
Mongolian spot
A similar kind of mole is observed in newborns, sometimes it occurs in adults, appearing on the skin in the form of a fifteen-centimeter spot in diameter as a result of a violation of the hormonal pigment. According to the name, this phenomenon is often recorded in Mongolia: in almost 92% of cases. The nevus is "located" on the sacrum or buttocks of the child. Transformation to melanoma is not observed. The stain may generally disappear over time.
fibroepithelial
This type of congenital or acquired nevus is often recorded. It appears under the influence of hormonal restructuring processes, in old age. Soft reddish/pinkish moles are large and can be localized throughout the body. Rarely transformed into malignant, easily removed. On their own, they cannot fall away.
Symptoms
Main hallmarks nevi is their appearance: shape, color, size. Some have hair follicles, roughness, warts and other "accompanying" elements. Others are smooth, localized, inconspicuous. Only a specialist is able to distinguish formations, give their descriptions, attribute them to certain groups and identify the danger with the help of diagnostic measures.
Diagnostics
The study of moles is an important point in the diagnosis, with the aim of identifying the danger of the transformation of benign nevus cells into malignant ones.
Diagnostics is carried out by the following methods:
- Visual, history taking. Asking questions to the patient, the doctor finds out:
- the period of formation of a nevus, whether it is congenital or acquired;
- whether changes in the appearance of education are noted;
- causes of the changes (burns, injuries, etc.);
- whether there was an attempt to remove a mole, in what way.
- A dermatoscope device that determines the nature of the origin, formation, location of nevus cells through the use of epiluminescent microscopy.
- Computed tomography, which allows to make an assessment of the structure, deep dimensions of birthmarks.
- Histological method, which determines tumor markers in the laboratory (after the operation to remove the nevus).
Important to remember! A timely visit to a dermatologist (at the first sign of transformation of a mole) for diagnosis can save a person's life, preventing the formation of a malignant tumor.
Biopsy for diagnostic purposes is not performed!
Treatment of nevi
A dermatologist-oncologist is engaged in the treatment of pigmented formations. The therapeutic approach is carried out in a clinical setting by the method of surgical intervention.
First of all, moles that are subject to regular injury or its risk and are located are taken into account:
- under hair;
- in women on the back, in the area of \u200b\u200bthe fastener of the bra;
- in men on the neck, face, chin (dangerous when shaving);
- in the inguinal region, skin folds;
- "on the leg" (they can tear or completely tear off).
To remove nevi, use the following methods:
- Resection. Nevus (usually large sizes) is excised along with three centimeters of the skin surrounding it with a scalpel under local anesthesia. The disadvantage of this type is the presence of a scar after surgery and soreness. The remote formation is undergoing histological examination.
- Cryodestruction. This is a procedure for freezing a nevus with liquid nitrogen. In this way, small formations can also be eliminated. The advantages of cryodestruction are the absence of scars and the need for additional anesthesia.
- Electrocoagulation. The nevus is cauterized with an electric current. Children undergo the procedure under general anesthesia, adults - under local anesthesia. Suitable for removing small and medium moles.
- Laser therapy. It is used to remove moles on the face, neck. With high precision, the laser does not leave scars on the skin. The main point of this procedure is the implementation of the depth of penetration of the laser beam under the skin to completely destroy the cells of the nevus.
Postoperative complications
The elimination of birthmarks does not always go smoothly, sometimes complications arise, consisting in:
- the development of the inflammatory process in cases of improper wound care in the postoperative period;
- malignancy (the process of formation of cancer cells) at the place where the nevus was not completely removed;
- cosmetic defect - the presence of a scar.
It's important to know! The method of surgical intervention is determined by the doctor, taking as a basis the features of the nevus, the functionality medical institution. The patient can express his wishes, but his opinion is not decisive.
Prevention of melanoma
To prevent the development of melanoma - a malignant formation - the influence of pathological factors should be excluded. Melanoma is dangerous because it can metastasize to the brain, liver, and other organs. Death from skin cancer occurs in 50% of cases.
Of course, the complete prevention of transformation into melanoma is impossible, but some recommendations, carefully followed, reduce the risk of degeneration of benign cells into cancerous ones.
Tips for:
- reducing the time spent under sunbeams, especially during periods
special activity (from 12 noon to 5 pm);
- avoidance of ultraviolet radiation affecting nevi;
- careful handling of moles so as not to injure them;
- timely appeal to a dermatologist-oncologist at the first signs of changes in moles regarding their shape, size, color.
Cosmetics designed to reduce the degree of influence of ultraviolet radiation on the skin are not able to protect nevi from harmful effects.
Moles are congenital or acquired skin defects formed as a result of the growth of a pigmented skin epithelial layer. That is, a mole is a kind of small formation that rises above the surface of the skin, has a different shape and is painted in brown or pink-red shades.
Mole - definition and main properties
Doctors name moles pigmented, melanocytic, melanoform or non-cellular nevi, since according to the mechanism of formation they are benign tumors originating from normal cells of various skin structures with the obligatory presence of melanocytes in them (cells that provide a brown or pinkish color to the mole). This means that the basic structure of a mole can be formed from cells in the epidermis (outer layer of the skin) or dermis (deep layer of the skin) that have formed a compact cluster in a small area. In addition to the structure-forming cells of the dermis or epidermis, a mole necessarily contains a small amount of melanocytes that produce a pigment that gives them a different color.Melanocytes are found in the skin of every person, with the exception of albinos, and provide a unique skin color by producing pigment. The pigment produced by melanocytes can vary from pink to dark brown. It is the color of the pigment produced by melanocytes that explains the different skin color in representatives of various peoples and ethnic groups. That is, if a person's skin is white, then melanocytes produce a light pink pigment, if dark, then light brown, etc.
Melanocytes that are part of the mole also produce a pigment of their usual, inherent color or shade (the same as on the areola of the nipples or labia minora). However, since the mole contains a rather large number of melanocytes per unit surface area, their pigment appears to be “concentrated”, as a result of which the color of the nevus is much darker than the rest of the skin. Therefore, in dark-skinned people, moles are usually painted in dark brown or almost black colors, and in owners of fair skin, nevi are pinkish or light brown.
Moles can be congenital or acquired. Congenital moles in children are not immediately visible, they begin to appear from 2 to 3 months of age. However, this does not mean that moles begin to form at 2-3 months, they are present from birth, just due to their very small size they are not visible. Moles grow with a person, increasing in size as the area of the skin increases. That is, while the child is very small, his congenital moles are also scanty and they are simply not visible. And when he grows up, his moles will increase in size so much that they can be seen with the naked eye.
Acquired moles appear in a person throughout life, and there is no age limit up to which nevi can form. This means that new moles on a person's skin can form until death. The most intensively acquired moles are formed during periods of hormonal changes - for example, puberty, pregnancy, menopause, etc. During these periods, old moles can grow, change color or shape.
Moles are benign neoplasms with, as a rule, a favorable course, that is, they do not tend to degenerate into. That is why in most cases they do not pose any danger and do not require treatment. However, in rare cases, moles can become malignant, that is, degenerate into skin cancer, and this is precisely their main potential danger.
However, it should not be assumed that every mole is a potential cancer growth site, since in 80% of cases skin cancer develops in an area of \u200b\u200bnormal and intact skin, on which there are no nevi. And only in 20% of cases, skin cancer develops as a result of malignancy of a mole. That is, a mole does not necessarily degenerate into cancer, moreover, this happens quite rarely, and therefore it is not worth treating each nevus as a future potential malignant tumor.
Moles - photo

These photographs show congenital moles.
This photo shows a nevus of Ota.



These photographs show various variants of pigmented moles.

This photo shows a "scattered" nevus.

This photo shows a halonevus (Setton's nevus).

This photo shows a blue (blue) mole.

This photograph shows a Spitz (Spitz) nevus.

This photo shows blue (Mongolian) spots.
Types of moles
Currently, there are several classifications of moles that distinguish different types and groups of nevi. Most often in practical medicine, two classifications are used: the first is histological, based on which cells the mole is formed from, and the second divides all nevi into melanoma-dangerous and melanoma-safe. Melanoma-dangerous are moles, which, theoretically, are capable of degenerating into skin cancer. And melanoma-safe are, respectively, those moles that under no circumstances degenerate into skin cancer. Consider both classifications and each type of moles separately.According to the histological classification, moles are of the following types:
1.
Epidermal-melanocytic moles (formed by epidermal cells and melanocytes):
- Borderline nevus;
- epidermal nevus;
- Intradermal nevus;
- Complex nevus;
- Epithelioid nevus (Spitz nevus, juvenile melanoma);
- Setton's nevus (halonevus);
- Nevus from balloon-forming cells;
- Papillomatous nevus;
- Fibroepithelial nevus;
- Verrucous nevus (linear, warty);
- Nevus sebaceous glands(sebaceous, seborrheic, Yadasson's nevus).
- Mongolian spots (spot of Genghis Khan);
- Nevus of Ota;
- Nevus Ito;
- Blue nevus (blue nevus).
- Dysplastic nevus (atypical, Clark's nevus);
- Pink melanocytic nevus.
- Combined nevus;
- Congenital nevus.
Border nevus
The border nevus is formed from a cluster of cells located on the border of the dermis and epidermis. Outwardly, it looks like a flat, slightly raised formation or just a spot on the skin, painted in dark brown, dark gray or black. Sometimes concentric rings are visible on the surface of the nevus, in the area of which the color intensity changes. The size of the borderline nevus is usually small - more than 2 - 3 mm in diameter. This type of mole is prone to degeneration into cancer, so they are considered dangerous.Epidermal nevus
An epidermal nevus is formed from a cluster of cells located in the surface layer of the skin (epidermis), and looks like a regular-shaped elevation, painted in various colors, from pinkish to dark brown. This type of mole can in rare cases degenerate into cancer, therefore it is considered potentially dangerous.Intradermal nevus
An intradermal nevus is formed from a collection of cells located in the deep layer of the skin (dermis). Externally, the nevus is a hemisphere, slightly rising above the surface of the skin and painted in dark shades - from brown to almost black. The size of an intradermal nevus is usually about 1 cm in diameter. This type of mole can degenerate into cancer in.Nevus of the sebaceous glands (sebaceous, seborrheic, nevus of Yadasson)
 The nevus of the sebaceous glands (sebaceous, seborrheic, nevus Yadasson) is a convex flat spot with a rough surface, painted in various shades of brown. A sebaceous nevus is formed in children due to a violation of the normal growth of various skin tissues. The causes of growth disorders of different skin tissues have not been elucidated, respectively, the exact causative factors of the sebaceous nevus are also unknown.
The nevus of the sebaceous glands (sebaceous, seborrheic, nevus Yadasson) is a convex flat spot with a rough surface, painted in various shades of brown. A sebaceous nevus is formed in children due to a violation of the normal growth of various skin tissues. The causes of growth disorders of different skin tissues have not been elucidated, respectively, the exact causative factors of the sebaceous nevus are also unknown. Such nevi are formed during fetal development, and appear on the skin of a child 2 to 3 months after birth. As the child develops, the sebaceous nevi grow, increase in size and become more and more prominent. Despite constant growth throughout life, Yadasson's nevus never transforms into cancer, so this type of mole is considered safe.
If a nevus bothers a person from a cosmetic point of view, then it can be easily removed. In this case, it is optimal to remove the mole after the child reaches the age of puberty.
Complex nevus
A complex nevus is a mole consisting of cells of the dermis and epidermis. Outwardly, a complex nevus looks like a small tubercle or a group of closely spaced tubercles.Epithelioid nevus (Spitz nevus, juvenile melanoma)
An epithelioid nevus (Spitz's nevus, juvenile melanoma) is a mole that is similar in structure to melanoma. Despite the similarity of the structure, Spitz's nevus is not a melanoma, it almost never becomes malignant, but its presence indicates a relatively high risk of skin cancer in this person.This type of mole usually appears in children under 10 years of age and grows quite quickly, increasing to 1 cm in diameter within 2 to 4 months. Spitz nevus is a convex formation of red-brown color and rounded shape with a smooth or bumpy surface.
Setton's nevus (halonevus)
Setton's nevus (halonevus) is a common brown mole surrounded by a wide rim of skin of a lighter shade compared to the color of the rest of the skin surface. Setton's nevi appear in people under 30 years of age.Over time, such a mole may decrease in size and become lighter, or completely disappear. After the disappearance of Setton's nevus, a white spot usually remains in its place, which persists for a long time - several months or even years.
These nevi are safe because they do not degenerate into cancer. However, people who have Setton's nevi on the skin have an increased tendency to autoimmune diseases, such as vitiligo, Hashimoto's thyroiditis, etc. In addition, a number of studies have found that the appearance of a large number of Setton's nevi is a sign of the development of skin cancer in some area of the skin.
Nevus from ballooning cells
A nevus of balloon-forming cells is a brownish spot or tubercle with a thin yellow rim. This type of mole very rarely degenerates into cancer.Mongolian spot
The Mongolian spot is a single spot or a group of spots on the sacrum, buttocks, thighs, or back of a newborn baby. The spot is painted in various shades of blue, has a smooth surface and slightly rises above the skin. The Mongolian spot develops due to the fact that the pigment produced by melanocytes is located in the deep layer of the skin (dermis), and not, as is normal, in the epidermis.Nevus of Ota
Nevus Ota is a single spot or a group of small spots on the skin, painted in blue. Spots are always located on the skin of the face - around the eyes, on the cheeks or between the nose and upper lip. Nevus Ota is a precancerous disease, as it tends to degenerate into skin cancer.Nevus Ito
The nevus of Ito looks exactly the same as the nevus of Ota, but is localized on the skin of the neck, above the collarbone, on the scapula, or in the region of the deltoid muscle. This type of nevi also refers to precancerous diseases.Blue nevus (blue mole)
A blue nevus (blue nevus) is a type of epidermal mole in which melanocytes produce a blue-black pigment. The nevus looks like a dense nodule, colored in various shades of gray, dark blue or black, and can be from 1 to 3 cm in diameter.Blue nevus, as a rule, is located on the back surfaces of the hands and feet, on the lower back, sacrum or buttocks. A mole is constantly growing slowly and is prone to degeneration into cancer, therefore it is considered dangerous. A blue nevus should be removed as soon as possible after it is identified.
Dysplastic nevus (atypical, Clark's nevus)
 Dysplastic nevus (atypical, Clark's nevus) is a single spot or a group of closely spaced round or oval spots with jagged edges, painted in light shades of brown, reddish or light red. In the center of each spot there is a small part protruding above the surface of the skin. An atypical nevus is larger than 6 mm.
Dysplastic nevus (atypical, Clark's nevus) is a single spot or a group of closely spaced round or oval spots with jagged edges, painted in light shades of brown, reddish or light red. In the center of each spot there is a small part protruding above the surface of the skin. An atypical nevus is larger than 6 mm. In general, moles are considered dysplastic if they have at least one of the following characteristics:
- Asymmetry (the mole has unequal contours and structure on different sides of the line drawn through the central part of the formation);
- Rough edges or uneven coloring;
- Size over 6mm;
- A mole is not like all the others on the body.
Papillomatous nevus
A papillomatous nevus is a type of common epidermal mole, the surface of which consists of bumps and outgrowths that resemble cauliflower in appearance.A papillomatous nevus always rises above the surface of the skin and consists of individual tubercles, colored brownish or pinkish in color and looking very unpleasant. When touched, the mole is soft and painless.
Despite the ugly appearance, papillomatous nevi are safe because they never degenerate into skin cancer. However, outwardly, these moles can be confused with malignant neoplasms skin, therefore, in order to distinguish such a nevus from cancer, a histological examination of a small piece taken using the biopsy technique should be performed as soon as possible.
Fibroepithelial nevus
Fibroepithelial nevus is very common and is a common epidermal mole, in the structure of which there are a large number of connective tissue elements. These moles have a round, convex shape, varying sizes, and are reddish, pinkish, or light brown in color. Fibroepithelial nevi are soft, elastic and painless, slowly growing throughout life, but almost never degenerate into cancer, and therefore are harmless.Pink melanocytic nevus
A pink melanocytic nevus is a common epidermal mole that is colored in various shades of pink or light red. Such moles are typical for people with very fair skin, because their melanocytes produce a pink pigment, not brown.Combined nevus
A combined nevus is a mole consisting of elements of a blue and a complex nevus.Verrucous nevus (linear, warty)
 Verrucous nevus (linear, warty) is a spot of an elongated, linear shape, painted in a dark brown color. This type of mole consists of normal cells, and therefore they almost never transform into skin cancer. Therefore, verrucous nevi are removed only when they create a visible and uncomfortable cosmetic defect.
Verrucous nevus (linear, warty) is a spot of an elongated, linear shape, painted in a dark brown color. This type of mole consists of normal cells, and therefore they almost never transform into skin cancer. Therefore, verrucous nevi are removed only when they create a visible and uncomfortable cosmetic defect. The causes of verrucous moles have not been established, but in most cases they are congenital. As a rule, these moles appear 2 to 3 months after birth or during the first 5 years of a child's life. Along with the growth of the child, the verrucous mole may increase slightly in size and darken, and also becomes more convex.
Congenital nevus (congenital mole)
A congenital nevus is a benign neoplasm that develops in a child some time after birth. That is, the causes of this type of moles are laid during fetal development, and the nevus itself is formed after the birth of the child.Congenital moles can have a different shape, size, edges, color and surface. That is, a mole of this species can be round, oval or irregular in shape, with clear or blurred edges, with a color that varies from light brown to almost black. The surface of a congenital mole can be smooth, warty, papular, folded, etc.
Congenital and acquired moles are almost indistinguishable in appearance. However, congenital moles are always larger than 1.5 cm in diameter. Sometimes such a nevus can be gigantic - more than 20 cm in diameter, and occupy the surface of the skin of an entire anatomical region (for example, chest, shoulder, neck, etc.).
All of the above nevi (moles) are also divided into two large groups, such as:
1.
Melanoma moles.
2.
Melanoma-safe moles.
Melanoma-dangerous moles are considered precancerous diseases, since they are the most often among all nevi that degenerate into malignant skin tumors. Therefore, they are recommended to be removed as soon as possible after they are identified. Melanoma-safe moles almost never degenerate into cancer, therefore they are considered safe, as a result of which they are removed only if there is a desire to eliminate a cosmetic defect associated with their presence on the skin.
Melanoma-prone moles include the following types:
- Blue nevus;
- Borderline nevus;
- Congenital giant pigment virus;
- Nevus of Ota;
- Dysplastic nevus.
Red moles
 A mole that looks like a small and convex red dot is a senile angioma. These angiomas are completely safe because they never turn into skin cancer.
A mole that looks like a small and convex red dot is a senile angioma. These angiomas are completely safe because they never turn into skin cancer. If the red mole is larger than the dot, then this formation may be a Spitz nevus, which in itself is safe, but is evidence that a person has an increased risk of skin cancer.
A red or pink bumpy mole in people over 45 can be a symptom of the early stages of skin cancer.
If the existing red mole does not grow, does not itch or bleed, then this is either a senile angioma or a Spitz nevus. If the mole actively increases in size, itches, bleeds and causes inconvenience, then most likely we are talking about the initial stage of skin cancer. In this case, you should immediately contact an oncologist who will conduct the necessary examinations and prescribe treatment.
hanging moles
By the term "hanging" moles, people usually mean some kind of formation that looks like a nevus, but is not tightly attached to the skin with a wide base, but, as it were, hanging on a thin leg. Such "hanging" moles can be the following formations:- Acrochordons- small skin-colored growths, usually located in the armpits, inguinal folds, on the neck or on the trunk;
- Convex growths of various sizes, painted in dark or flesh colors and having a smooth or bumpy surface, may represent epidermal nevi or keratosis.
If the "hanging" mole turned black and became painful, then this indicates its torsion, malnutrition and blood supply. Usually, soon after blackening and the development of soreness, the "hanging" mole disappears. Such an event is not dangerous and does not provoke the growth of new similar moles. However, in order to ensure optimal healing of the skin and remove, if necessary, blood clots or remnants of dead tissue, you should consult a doctor after falling off the "hanging" mole.
If at some point a person has a lot of acrochordons ("hanging" moles), then he should take a blood test for glucose concentration, since such an event is often a sign of developing. That is, from the point of view of skin cancer, the appearance of a large number of "hanging" moles is not dangerous, but this indicates the development of another serious disease.
big mole
Moles are considered large if their largest size is more than 6 mm. As a rule, such large moles are safe, provided that their structure does not change and the size does not increase over time. Only large, dark-colored (gray, brown, black-purple) moles are dangerous, as they can degenerate into melanoma (skin cancer).However, in order to fully verify the safety of a large mole on the skin, you should consult a dermatologist who can examine it, perform dermatoscopy and take a biopsy. Based on the manipulations performed, the doctor will be able to accurately determine the histological type of the mole and, thereby, determine the degree of its danger. Such an examination will allow a person to make sure that the mole he has is safe and, thereby, provide peace of mind in the future, which is very important for an acceptable quality of life.
Lots of moles
 If a person has a lot of moles within a relatively short period of time (1 - 3 months), then he should definitely consult a dermatologist to determine what type of nevi belong to.
If a person has a lot of moles within a relatively short period of time (1 - 3 months), then he should definitely consult a dermatologist to determine what type of nevi belong to. In the vast majority of cases, the appearance of a large number of moles is not dangerous, since it is a skin reaction to sunburn or other factors. environment. However, in some rare cases, a large number of moles may indicate serious and serious illnesses skin or immune system, as well as malignant tumors in the internal organs.
Dangerous moles
Moles that can degenerate into cancer or look very similar to a malignant tumor are considered dangerous. If a mole is prone to cancerous degeneration, then it is actually a matter of time when it becomes not a benign, but a malignant formation. That is why doctors recommend removing such moles.If the mole is outwardly similar to cancer, as a result of which they cannot be distinguished, then it should be removed without fail and as soon as possible. After removing the mole, it is sent for a histological examination, during which the doctor examines the tissues of the formation under a microscope. If the histologist gives a conclusion that the removed mole is not cancer, then no additional therapeutic measures are needed. If, according to the conclusion of histology, the remote formation turned out to be a cancerous tumor, then you should undergo a course of chemotherapy, which will destroy the tumor cells present in the body and, thereby, prevent a possible relapse.
Currently classic The following are considered signs of a dangerous mole:
- Pain of a different nature and degree of intensity in the area of a mole;
- Itching in the area of the mole;
- Visible increase in the size of the mole in a short time (1 - 2 months);
- The appearance of additional structures on the surface of the mole (for example, crusts, sores, bulges, bumps, etc.).
In practice, doctors believe that the most accurate sign of a dangerous mole is its dissimilarity to other moles that a person has. For example, if a person has moles with uneven edges and uneven coloring, which seem dangerous, but exist for many years and do not cause concern, then a beautiful and even mole that appears among these "suspicious" nevi, which is considered completely normal according to classical criteria, will be dangerous. And, accordingly, on the contrary, if among a large number of even and regular moles one of a strange shape and uneven color appears, then this particular mole will be dangerous. This method of identifying a dangerous formation is called the ugly duckling principle.
AT general view this principle The ugly duckling, which can be used to distinguish the malignant degeneration of a mole, is that cancer is a mole that is not like the others on the body. Moreover, either a newly appeared, unusual and different mole is considered dangerous, or an old one that suddenly changed, began to grow, itch, itch, bleed and acquired an unusual appearance.
Thus, moles that have always had an unusual appearance and do not change it over time are not dangerous. But if suddenly an old mole began to actively change, or a new nevus appeared on the body, different from all the others, then they are considered dangerous. It means that moles with the following symptoms:
- Rough or blurry edges;
- Uneven coloration (dark or white spots on the surface of the mole);
- Dark or white rims around the mole;
- Black dots around the mole;
- Black or blue color of the mole;
- Asymmetry of a mole
In addition, a subjective criterion for a dangerous mole is that a person suddenly at some point begins to feel and feel it. So many people point out that they began to literally feel their mole, which began to degenerate into cancer. Many practicing dermatologists attach great importance to this seemingly biased sign, since it allows you to detect cancer at an early stage.
mole grows
Normally, moles can slowly grow up to 25-30 years, while growth processes continue throughout the human body. After the age of 30, moles usually do not increase in size, but some of the existing nevi can grow very slowly, increasing by 1 mm in diameter over several years. This growth rate of moles is normal and is not considered dangerous. But if the mole begins to grow faster, significantly increasing in size within 2 to 4 months, then this is dangerous, since it may indicate its malignant degeneration.Mole itches
 If a mole or the skin surrounding it begins to itch and itch, then this is dangerous, as it may indicate a malignant degeneration of the nevus. Therefore, if itching appears in the area of the mole, it is necessary to consult a doctor as soon as possible.
If a mole or the skin surrounding it begins to itch and itch, then this is dangerous, as it may indicate a malignant degeneration of the nevus. Therefore, if itching appears in the area of the mole, it is necessary to consult a doctor as soon as possible. If the skin surrounding the mole begins to peel off with or without itching, then this is dangerous, as it may indicate an early stage of malignant degeneration of the nevus.
If the mole began not only to itch and itch, but also to grow, change color or bleed, then this is an undoubted sign of malignancy of the nevus and requires urgent medical attention.
mole bleeds
If a mole began to bleed after an injury, for example, a person scratched it, tore it, and so on, then this is not dangerous, since it is a normal reaction of tissues to damage. But if the mole bleeds for no apparent reason constantly or periodically, then this is dangerous and in such a situation it is necessary to consult a doctor.Reasons for the appearance of moles
Since moles are benign tumors, possible reasons their appearance may be various factors that provoke active and excessive division of skin cells in a small and limited area of \u200b\u200bthe skin. So, it is now believed that these possible causes of the development of moles may be the following factors:- Defects in the development of the skin;
- genetic factors;
- Ultraviolet radiation;
- Skin injury;
- Diseases accompanied by hormonal imbalance;
- Prolonged use of hormonal drugs;
- Viral and bacterial, occurring for a long time.
Genetic factors are the cause of moles that are inherited from parents to children. As a rule, any characteristic birthmarks or large moles located in strictly defined places are transmitted in this way.
UV radiation stimulates the active production of melanin, which colors the skin in a darker color (tan) and thus protects it from negative effects. solar radiation. If you are in the sun long time, then the process of intensive reproduction of melanocytes - cells that produce melanin - will start. As a result, melanocytes will not be able to be evenly distributed in the thickness of the skin and form a local accumulation that will look like a new mole.
Injuries are indirectly the causes of the formation of moles. The fact is that after an injury in an area with impaired tissue integrity, a large number of biologically active substances are formed. active substances that stimulate the regeneration process. Normally, as a result of regeneration, the integrity of tissues after an injury is restored. But if the regeneration is excessive, proceeding under the influence of a large number of biologically active substances, then the process does not stop in a timely manner, as a result of which a small amount of "extra" tissues is formed, which become moles.
Hormonal imbalance can provoke the formation of moles due to an increase in the production of melanotropic hormone. Under the influence of this hormone, the process of reproduction of melanocytes and other cells is activated, from which moles can form.
Viral and bacterial infections provoke the formation of moles due to traumatic damage to the skin that occurs locally, in the area of the infectious-inflammatory process.
Moles in children
In children, moles can appear from 2 to 3 months. Up to the age of 10, the appearance of moles in a child is considered normal and does not pose any danger. Moles that appear before 10 years old will slowly increase in size until 25 - 30 years old, while the person himself continues to grow. In all other respects, moles in a child are no different from those in adults.Moles and warts in children: risk factors and prevention of nevus degeneration into cancer, signs of malignancy, mole injuries, treatment (removal), answers to questions - video
Moles in women
 Moles in women do not have any fundamental features and have all general characteristics and the properties described in the previous sections. The only feature of moles in women is that during puberty, new ones can actively appear and old ones grow. During pregnancy and lactation, moles do not undergo any fundamental changes. Therefore, if a mole begins to grow or change in any way in a pregnant woman or a nursing mother, then you should consult a doctor.
Moles in women do not have any fundamental features and have all general characteristics and the properties described in the previous sections. The only feature of moles in women is that during puberty, new ones can actively appear and old ones grow. During pregnancy and lactation, moles do not undergo any fundamental changes. Therefore, if a mole begins to grow or change in any way in a pregnant woman or a nursing mother, then you should consult a doctor. Removal of moles
Removal of moles is a method of eliminating the danger associated with the likelihood of their degeneration into cancer. Therefore, moles that have a potential danger should be removed.Is it possible to remove nevi (remove moles)?
Often, wanting to remove one or more moles, people ask themselves: "Is it possible to remove these moles and will it cause any harm?" This question is logical, since at the household level there is a widespread opinion that it is better not to touch moles. However, from the standpoint of the likely development of skin cancer, the removal of any mole is completely safe. This means that the removal of a mole cannot contribute to the development of skin cancer. Therefore, you can safely remove any mole that causes discomfort or creates a cosmetic defect.Any operations to remove moles are safe, since complications during their implementation are extremely rare and, in most cases, are associated with allergic reaction for pain medication, bleeding, etc.
What moles should be removed?
Moles that look like skin cancer or have begun to change actively in recent months (grow, bleed, change color, shape, etc.) are subject to removal. Such moles should be removed as soon as possible in order to prevent possible tumor progression and the transition of malignant pathological process to more severe stages.At the same time, it is not necessary to remove all moles that are on the body and cause any suspicion of their possible malignant degeneration in the future, since this is not rational and ineffective from the standpoint of preventing skin cancer. Indeed, in most cases, skin cancer develops from a completely normal area of \u200b\u200bthe skin, and not from a mole, the malignancy of which is extremely rare. Therefore, it is not necessary to remove all suspicious moles, it is better to leave them on the body and regularly visit a dermatologist for their preventive examination.
In addition, you can remove any moles that do not satisfy a person for aesthetic reasons, that is, they create a visible cosmetic defect.
Methods for removing moles (nevi)
Currently, moles can be removed using the following methods:- Surgical removal;
- laser removal;
- Removal with liquid nitrogen (cryolysis);
- Electrocoagulation ("cauterization" by electric current);
- radio wave removal.
All other moles can be removed with a laser or liquid nitrogen, which allow the manipulation to be carried out as carefully and bloodlessly as possible.
Surgical removal
Surgical removal of a mole consists of cutting it out with a scalpel or a special tool (see Figure 1).

Picture 1- Tool for removing moles.
For the operation, the mole itself and the skin around it are treated with an antiseptic (alcohol, etc.). Then, a local anesthetic is injected into the thickness of the skin under the mole, for example, Novocaine, Lidocaine, Ultracaine, etc. Then, incisions are made on the sides of the mole, through which it is removed. When using a special tool, it is installed above the mole and immersed deep into the skin, after which the cut tissue area is removed with tweezers.
After removal of the mole, the edges of the wound are pulled together with 1-3 sutures, treated with an antiseptic and sealed with a plaster.
Laser removal
Laser mole removal is the evaporation of a nevus with a laser. This method is optimal for removing superficial age spots. Laser removal of moles provides minimal tissue trauma, as a result of which the skin heals very quickly and a scar does not form on it.Removal with liquid nitrogen
 Removal of a mole with liquid nitrogen is the destruction of a nevus under the influence of low temperature. After the mole is destroyed by liquid nitrogen, it is removed from the tissues with tweezers or cut out with a scalpel. The method of removing a mole with liquid nitrogen is not easy, since it is impossible to control the depth of tissue destruction. That is, if the doctor retains liquid nitrogen on the skin for too long, this will lead to the destruction of not only the mole, but also the surrounding tissues. In this case, a large wound will form, which is prone to prolonged healing and scarring.
Removal of a mole with liquid nitrogen is the destruction of a nevus under the influence of low temperature. After the mole is destroyed by liquid nitrogen, it is removed from the tissues with tweezers or cut out with a scalpel. The method of removing a mole with liquid nitrogen is not easy, since it is impossible to control the depth of tissue destruction. That is, if the doctor retains liquid nitrogen on the skin for too long, this will lead to the destruction of not only the mole, but also the surrounding tissues. In this case, a large wound will form, which is prone to prolonged healing and scarring. Electrocoagulation
Electrocoagulation of a mole is its destruction with the help of an electric current. This method is commonly referred to as "cauterization". Many women are familiar with the essence of this method if they have ever "cauterized" cervical erosion.Radio wave mole removal
Radio wave mole removal is an excellent replacement for the surgical method, which is more traumatic. Radio wave removal of a mole is as effective as surgical removal, but less traumatic. Unfortunately, this method is rarely used due to the lack of the necessary equipment.Moles (nevi): causes of appearance, signs (symptoms) of degeneration into skin cancer, diagnosis (dermatoscopy), treatment (removal), prevention of malignancy - video
Moles (nevi): signs of dangerous and non-dangerous moles, risk factors for degeneration into cancer, methods for diagnosing and removing moles, doctor's advice - video
Mole removal by radio wave surgery - video
Removed mole
A few hours after the removal of the mole, pain of varying degrees of intensity may appear in the wound area, due to a violation of the integrity of the skin structures. These pains can be stopped by taking drugs from the group of non-steroidal anti-inflammatory drugs (NSAIDs), such as Paracetamol, Nurofen, Nimesulide, Ketorol, Ketanov, etc.The wound itself does not require any special care or treatment until the sutures are removed, which is done on days 7-10. After that, to accelerate healing and prevent scar formation, it is recommended to lubricate the wound with Levomekol, Solcoseryl or Methyluracil ointments.
Until the wound heals completely, so as not to provoke inflammation, infection and the formation of a rough scar, the following rules should be followed:
- Do not apply cosmetics to the wound;
- Do not tear or wet the crust;
- Cover the wound with a cloth or band-aid from exposure to sunlight.
In rare cases, the wound after the removal of the mole may become inflamed due to the ingress of pathogenic bacteria into it, which will lead to longer healing and scar formation. Signs of an infection are as follows:
- wound inflammation;
- The pain in the area of the wound became stronger;
- Pus in the area of the wound;
- Dispersed edges of the wound.
In rare cases, the sutures may diverge, as a result of which the edges of the wound diverge to the sides and slowly grow together. In such a situation, you should consult a doctor so that he puts in new stitches or pulls the existing ones tighter.