Low AMH – diagnosis of infertility. Anti-Mullerian hormone for assessing ovarian reserve - what is it? If amg is low, is it possible to do eco?
I'll start from afar. I was shown IVF due to the absolute tubal factor, the tubes were removed in 2012, I won’t tell you about the pandemonium that preceded all this. In the fall of 2015, after hearing a lot of praise about the head of the Clinic for Reproductive and Prenatal Medicine EMC Yu. Voznesenskaya, we went to see her. I was taken into a short protocol, which resulted in one 2-day-old embryo and it was implanted in me, of course, it did not take root, and then I decided to look more carefully for a qualified doctor and dived into more detail...
IVF with DU for low AMH + external endometriosis
Dear ladies :), girls, “colleagues”, help me collect information about the successful (and maybe not so successful) results of IVF with DU for low AMH and external endometriosis. Due to endometrioid cysts, my left appendages (ovary + tube) were first removed, and after 4 years, a resection of the right ovary was performed. Accordingly, my AMH has dropped significantly, now it is 0.11 ng/ml, FSH = 11.69 mIU/ml. I have been on HRT for about 2 years - I take Femoston 2/10. I had a hysteroscopy in 2014 - everything inside the uterus was normal. But IVF...
The inability to naturally conceive a baby on your own is often associated with hormonal imbalances in a woman. Among the great variety of endocrine disorders, AMH deficiency stands out. The level of this hormone is extremely important for the reproductive function of both men and women, but it “works” differently in representatives of different sexes.
Before IVF, an AMH test is mandatory. What should the Mullerian inhibitor standards be, is it possible to get pregnant in an IVF protocol with a low level of this substance, and how to increase the concentration of AMH, we will tell you in this article.

What it is?
AMH (anti-Müllerian hormone) was discovered back in the 19th century, when protein molecules that affect growth processes in the organs of the reproductive system were discovered by the German naturalist and biologist Johann Muller. He found that embryos, regardless of gender, have a common feature - a tube-canal, from which, at approximately the 9th week of pregnancy, epididymis are formed in male embryos under the influence of AMH. This is how sexual differentiation occurs.
In female embryos, AMH is not produced and by default the canal-tube begins to form into the fallopian tubes and ovaries. In girls, AMH begins to be produced only after birth.
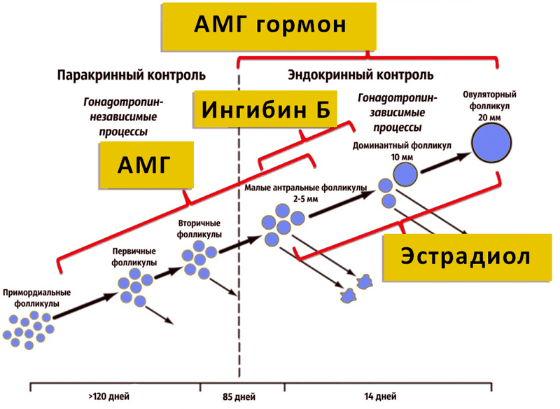
The functions of the Mullerian inhibitor are to ensure human sexual function throughout life. In women, the AMH level indicates the functioning of the ovaries and the maturation of the egg. Mullerian inhibitor regulates follicular growth and its concentration decreases with age. The amount of AMH in a woman’s blood plasma is a fairly accurate indicator of the ovarian reserve; it can indicate the approximate number of eggs that remain “in reserve”.
Before puberty in girls, AMH is detected in extremely low concentrations. With the onset of puberty, the level of Müller inhibitor begins to increase, and then gradually decreases throughout life. During menopause, AMH is not detected in blood plasma.
AMG norms for IVF
As already mentioned, the concentration of Müller inhibitor in the blood plasma is directly proportional to age. Therefore, the norms depend on how old the patient is at the time of planning the in vitro fertilization protocol. The norm for women under 35 years of age is 4.0-6.5 ng/ml. The level of AMH is considered slightly disturbed at levels of 2.5-4.0 ng/ml. An indicator of 0.3-2.2 ng/mg is considered reduced. Concentrations less than 0.3 ng/ml are considered low levels.
For women over 35 years of age, the norms are different. The normal level is considered to be 1.5-4.0 ng/ml. An indicator of 1.0-1.3 ng/ml can be considered conditionally normal. A low level is 0.5-1.0 ng/ml, and a critical decrease is considered to be less than 0.5 ng/ml.

These normative values are typical for women whose infertility is caused not by hormonal disorders, but, for example, by obstruction of the fallopian tubes or thinning of the endometrium. But in most cases, women with endocrine disorders or concomitant endocrine problems have to resort to IVF, and therefore the minimum standard AMH value for IVF is 0.6-0.8 ng/ml.
On average, for in vitro fertilization, the AMH concentration is required to be from 0.6 ng/ml to 2.4 ng/ml.
Women who took oral contraceptives for a long time before planning pregnancy most often suffer from low levels of anti-Mullerian hormone, since such drugs suppress the production of AMH and lead to premature menopause.

Deviations from norms and pregnancy prognosis
A high AMH level before the IVF procedure should alert the attending physician. Patients whose Müller inhibitor concentration is increased to 6.5-7 ng/ml are more likely to develop ovarian hyperstimulation syndrome, a dangerous complication of the first stage of in vitro fertilization. High levels of the hormone slow down or completely block the growth of follicles, therefore, obtaining the required number of eggs for in vitro fertilization will not be easy.
When anti-Mullerian hormone levels are low, the chance of pregnancy decreases because few follicles are formed. If laboratory values are below normal at the protocol planning stage, the doctor may assume that the ovarian response to hormonal stimulation of superovulation will be weak.

Low AMH levels reduce the likelihood of pregnancy even during IVF with ICSI, when the sperm is injected under the oocyte membrane using a thin hollow needle. A reduced level of a hormonal substance indicates low quality of eggs, and therefore, even if pregnancy occurs as a result of an IVF protocol, the likelihood of a miscarriage or frozen pregnancy in the early stages will be high.
Hormone concentration indicators must be taken into account when choosing the nature of the protocol. If the AMH level in a woman’s blood plasma is below 0.71 ng/ml, stimulation is carried out with high doses of antagonists in combination with FSH. If the concentration of the hormone in a woman’s blood is higher than 0.71 ng/ml, but does not exceed 2.1 ng/ml, then a long protocol is usually prescribed, in which hormones that suppress ovulation and cause artificial menopause will be used first, and then follicle-stimulating hormones .

The probability of conception with successful IVF and increased AMH levels is higher than with reduced concentrations. The lower the values, the more difficult it is for a woman to become pregnant, even after embryo transfer. In general, the success rate of an IVF protocol in Russian clinics is estimated at 35-45%. With a significant decrease in AMH, the predicted probability of successful pregnancy does not exceed 25-30%. There is a chance of pregnancy if a woman does not have other concomitant pathologies of the uterus, cervix, or endometrium.
Low AMH levels in the natural cycle do not exclude the possibility of pregnancy, but make it even less likely. Without appropriate preliminary therapy, IVF in a natural cycle with such indicators is avoided.

It is always important to establish the true cause of the decrease in Muller inhibitor, so that before any IVF protocol, the woman can undergo targeted treatment of the pathology.
How to get tested correctly?
A sample of a woman's venous blood is used for the study. As directed by a gynecologist, reproductive specialist or endocrinologist, a woman should contact the laboratory on days 3-5 of the menstrual cycle. It is during this period of time that the AMH indicator is most adequate.
The AMH level is extremely unstable, and therefore you need to prepare for the blood test in advance - reduce physical activity a week before visiting the clinic, get a good night's sleep, and prevent your health from deteriorating. Any illnesses you have had in the last 2-3 weeks, as well as taking antibiotics or anticonvulsants, can lead to distorted test results.
The stress and emotional turmoil that a woman experiences leads to fluctuations in the level of anti-Mullerian hormone. 10-12 hours before you should avoid eating, 3 hours before you should not drink water. A few hours before donating blood, it is advisable not to smoke or drink strong tea or coffee.
On average, the test result becomes known after 48 hours. In some laboratories, the test takes about a day.

Is it possible to increase AMH?
Since the concentration of Müllerian inhibitor is unstable, it can vary - rise and fall depending on many factors. For example, in summer and spring, the level of the hormone in a woman’s body increases by about 15-18%. Therefore, it is often associated with vitamin D, which is produced when human skin comes into contact with sunlight.
DHEA (dehydroepiandrosterone) therapy is considered effective. This hormonal treatment is prescribed for very low AMH levels 3-4 months before IVF. In most cases, in combination with vitamin D, hormonal treatment gives a positive result, and AMH tests before the IVF protocol show higher levels of anti-Mullerian hormone.
Sometimes doctors recommend that women take the anti-menopausal drug Melsmon. It is produced in Japan based on placental cells. Like any other product in the placentotherapy line, the drug has its advantages and disadvantages, but often the effect of taking it is significantly exaggerated by the manufacturers.


In 2018, changes occurred in the legislation, and the IVF procedure became available through general health insurance (CHI). Unfortunately, according to the norms, not all women who are unable to conceive a child naturally can take advantage of this right. The patient must meet a number of criteria, including the level of anti-Mullerian hormone (AMH), which is responsible for the likelihood of a positive outcome of artificial insemination.
You can perform the in vitro fertilization procedure at your own expense regardless of almost any test results. The doctor can warn, but cannot refuse to conceive in this way. If a woman wants to exercise the right to have her situation considered for a quota, she must be prepared to be refused, due to the unpromising nature of this procedure.
What should be the norm for women's anti-Muller index?
Anti-Mullerian hormone (AMH), also sometimes called Müllerian inhibitory substance. This hormone is tested in patients to determine the likelihood of their pregnancy: the higher it is, the more likely a woman is to become pregnant. For 2018, this indicator must be at least 1.0 to receive a quota for IVF.
It is given only to those women who have sufficient levels of the hormone, and therefore a high chance of conception. Such measures are aimed at preserving budgetary funds by excluding from the queue for the quota patients whose artificial insemination most likely will not end positively.
AMH allows you to diagnose reproductive health problems in a woman
It is necessary to clarify that in some regions the value of the minimum possible AMH level for IVF may differ from the general one in the country. Information about the situation in your region should be clarified at the reproductive center of your city or at the local antenatal clinic.
AMH promotes tissue growth during embryonic development and, based on its value, a specialist is able to fairly accurately predict the number of eggs that will be capable of fertilization. The concentration of anti-Mullerian hormone depends on the number of dormant follicles, and reproductive potential can be determined from them.
Its norm for patients of reproductive age can be from 1.0 to 2.5 ng/ml, which indicates the woman’s ovarian reserve. It happens that the AMH value can reach up to 15 nanograms per milliliter; with such indicators, IVF at the expense of compulsory medical insurance will also be denied.
In cases where the AMH level is above 0.6669 ng/ml, but below 1.0, a woman has a small chance of fertilizing her own egg and she can go to a private clinic, where doctors will select the necessary IVF protocol for her.
Features of the procedure with low hormone levels
In patients whose AMH level does not reach the minimum norm, too little follicular growth is expected, as well as an insufficient response to stimulation. Also, according to research results, it has been proven that if the anti-Mullerian level shows little of the hormone, it can lead to various pathologies of embryo development.

Anti-Mullerian hormone values
Women who want to undergo IVF under compulsory medical insurance need to be prepared for the fact that until the AMH level is 1 or higher, the commission will refuse to receive a quota. If the level of Müller inhibitory substance is zero or fluctuates around this level, ovarian stimulation is pointless. It must be said that during the fertile period, the AMH value remains practically unchanged.
IVF protocol
If AMH levels are low, the following IVF protocols can be used:
- Japanese protocol– stimulation is minimal and intermittent; in each cycle, specialists try to obtain 1-2 eggs capable of fertilization. All obtained embryos undergo cryopreservation and are transferred in subsequent cycles;
- eco in natural cycle– ovulation stimulation is not carried out, or it is prescribed in a minimal amount. Over several cycles, specialists try to obtain at least one egg.
Patients with low ovarian reserve can be prescribed hCG and LH drugs, estrogens, androgens, L-arginine, herbal medicine, as well as improving microcirculation and even hirudotherapy. All these procedures and drugs are not included in compulsory medical insurance, but after their use, positive dynamics are observed, and the chances of a successful outcome of IVF increase.
The patient's AMH level will influence the reagents used to stimulate ovulation.
In vitro fertilization without hormonal therapy
For patients whose Müllerian inhibitory substance level is less than normal, a suitable IVF protocol will be used in their natural cycle. This is done in cases where hormonal drugs are contraindicated for a woman who is unable to conceive naturally, or in a situation where the growth of more than one follicle is not expected as a result of stimulation.
IVF without hormonal therapy is carried out mainly for patients older than reproductive age, that is, up to 30 years old, as well as for women with a low ovarian cycle. An embryo obtained from a single high-quality fertilized egg can be subjected to a cryoprotocol or transferred in a fresh cycle. There is also the practice of transferring embryos accumulated in natural cycles into the uterine cavity.
The patient undertakes all examinations, additional appointments with a specialist, as well as tests. IVF under compulsory medical insurance only includes: primary appointment with a reproductive specialist, ovulation stimulation.
Low AMH and high FSH levels
In addition to a sufficient AMH value, when taking tests for IVF, it will be necessary to find out what level of follicle-stimulating hormone of the pituitary gland (or FSH). The production of FSH stimulates the growth of follicles and eggs. If AMH is low, FSH usually increases, which has an adverse effect on conception: the quality of the eggs is insufficient for fertilization.

Estimated AMH content in men and women depending on age
In this situation, the IVF procedure is impossible, or a donor egg must be used. Unfortunately, in 2018, the use of donor material is not included in compulsory medical insurance and the patient will have to pay all expenses herself. An FSH level of more than 10 nanograms per milliliter is considered high.
If both AMH and FSH values are low, then there is still a small chance of conception. The artificial insemination procedure will be carried out with minimal stimulation and if there is a chance of obtaining a few cells.
conclusions
- A woman's reproductive potential depends on the level of AMH. Based on its concentration, a specialist can determine the number of eggs capable of fertilization.
- For 2018, the AMH value for IVF according to compulsory medical insurance should be no less than 1.0 and no more than 2.5 ng/ml, although in each individual case the decision on the quota is made individually.
- For women with low levels of anti-Mullerian hormone, the Japanese protocol and the IVF protocol in a natural cycle can be applied. Also, they may be prescribed various hormonal medications and procedures aimed at improving microcirculation.
- In vitro fertilization in the natural cycle is used mainly for patients over 30 years of age, as well as for those for whom hormonal medications are contraindicated.
- If the FSH level is more than 10 ng/ml, IVF is impossible.
Due to the current development of careerism propaganda, many married couples under 40 do not even think about realizing their reproductive function. They consider the priority task to be successful as an individual, as a specialist in any industry, and only then as parents. But when they want to get pregnant, they may not be able to do so due to various disorders of the reproductive system.
And some people for many years, and sometimes even decades, make futile attempts to get pregnant, but with no effectiveness.
Whether during natural conception or when using assisted reproductive technologies, an important indicator is the age component, since with age the ovarian reserve of the ovaries is depleted and the ovaries give a poor response to stimulation, at a certain point conception will no longer be possible. Also, with age, the physiological compensatory capabilities of the body decrease, and the risk of genetic abnormalities increases when performing extra-sacorporeal fertilization.
IVF and AMG
To identify the ovarian reserve in modern medicine, they use the determination of such an indicator as anti-Mullerian hormone (AMH).
What is anti-Mullerian hormone? This is an indicator of the reproductive capacity of a particular woman. The hormone is produced by the ovarian follicles of the female body, whose diameter is less than 4 mm, throughout the period of a woman’s life from birth to menopause. The production of anti-Mullerian hormone is not affected by other hormonal fluctuations, so its level is stable throughout a woman’s menstrual cycle. AMH is the first marker that can indicate the aging of one of the main reproductive organs - the ovaries. Even if a woman’s cycle has not yet undergone any changes, the level of this hormone can already indicate ovarian depletion.
AMG level and norms for eco
AMH for IVF: the acceptable value at which the in vitro fertilization procedure can be performed is an AMH level of no less than 0.8 ng/ml. If this level is lower than this indicator, then the quality of the obtained eggs is considered questionable.
Average levels of anti-Mullerian hormone are from 1 to 12 ng/ml. these indicators indicate a high ovarian reserve.
Recommended days for diagnosis are days 3-5 of the menstrual cycle. Before taking the test, you must refrain from eating for 8 hours; water is allowed. You should also refrain from physical activity on the eve of the examination. Blood donation takes place from 8 to 11 am. AMH decreases after IVF.
Is it possible to perform IVF with low AMH?
During a set of diagnostic measures, it is mandatory to determine the level of anti-Mullerian hormone. If, upon receipt of examination data, the AMH level is less than 1.0 ng/ml, then it can be concluded that poor performance can be expected when ovulation is stimulated during an in vitro fertilization protocol.
Statistical data based on an analysis of the relationship between the level of anti-Mullerian hormone and the outcomes of the use of assisted reproductive technologies indicate lower rates of good outcomes from the use of IVF in women with low AMH.
In addition to anti-Mullerian hormone, there are a number of markers that also indicate low ovarian reserve. Among them are:
- Age indicator – women over 40 years old;
- Ovarian sizes: ovaries measuring less than 3 cm cubic are not favorable in terms of high reserve;
- Follicle-stimulating hormone value equal to more than 15 IU/ml;
In what situations should women undergo this examination:

- Diagnosis of infertility;
- The presence of failures when applying the in vitro fertilization protocol;
- Presumptive diagnosis of polycystic ovary syndrome.
There are a number of factors that can cause a woman’s ovarian reserve to be reduced:
- Surgical interventions, the essence of which is resection of part of the ovary, removal of the ovary;
- The use of radiation therapy, chemotherapy;
- Autoimmune pathologies;
- Genetic reasons for decreased reserve;
- IVF and low AMH.
In pathological conditions such as low AMH levels, so-called “soft” protocols are used for IVF.
The Japanese Protocol is widely used. This regimen is used when anti-Mullerian hormone levels are less than 1 ng/ml. The essence of this technique is the use of low doses of drugs to stimulate ovulation using breaks between doses. The main task is to obtain at least a few healthy, high-quality eggs for fertilization and their cryopreservation. They are transferred in the following cycles.
Also, for the purpose of carrying out extracorporeal fertilization, a short protocol is used, which is carried out when the anti-Mullerian hormone decreases to at least 0.5 ng/ml and normal indicators of the age criterion, the level of follicle-stimulating hormone, and a good number of antral follicles.
There are methods for preparing women to use assisted reproductive technologies. These include the use of androgens in the form of transcutaneous testosterone, which improves the production of hormones in granulosa cells, the use of human chorionic gonadotropin, luteinizing hormone, and the possible use of aromatase inhibitors - Letrozole. Hirudotherapy has proven itself well in the practice of reproductive medicine.
In reproductive medicine, it is necessary to predict the development of ovarian tissue depletion. To do this you need:
- Scrupulously collect anamnestic data;
- Collect a thorough family history;
- A laboratory diagnostic examination is required in the form of determination of AMH, FSH, LH;
- Conducting high-precision ultrasound diagnostics to determine the number of antral follicles;
- Genetic analysis to identify genes for premature ovarian failure.
If such an analysis reveals significant risks to a woman, then they should be advised to quickly use their reproductive potential. It is necessary to convey to the woman that with a low ovulatory reserve, the chances of getting pregnant are less and less every month and not every month in this situation ovulation occurs, which also reduces the chances of spontaneous pregnancy.
Eco with low AMH and high FSH

With the development of modern methods of reproductive medicine, a new technology for banking oocytes or embryos obtained in several natural cycles has appeared. By cryopreservation, these cells or embryos create a bank of biomaterial, which is subsequently used during the IVF protocol. When planning radiation or chemotherapy, if a woman has low AMH, IVF can be performed using cryopreservation of the material before these manipulations.
IVF can also be performed in the EC with low AMH, that is, the in vitro fertilization protocol is carried out without the use of harsh hormonal stimulation of the ovaries. An egg is used that has matured on its own in a woman’s normal ovarian-menstrual cycle. And the cost of this procedure is significantly less than the protocol with stimulation of ovulation with hormonal drugs.
IVF with low AMH and high FSH, the issue may be resolved in favor of using donor eggs, since the quality of the eggs may be questionable. According to statistics, the eggs of women under 35 years of age and after 35 were studied and the following results were obtained, which describe the data that in such embryos obtained from fertilization of the eggs of women over 35 years of age, there is an increased risk of chromosomal aberrations in the form of Down syndrome, Shereshevsky-Turner syndrome. To exclude such pelagic conditions, there is the only reliable method of preimplantation genetic diagnosis, which makes it possible to exclude the transfer of embryos with any genetic pathologies.
IVF and high AMH

What to do when the level of anti-Mullerian hormone is not lower, but higher than the borderline norm?
There are two main reasons for increased levels of this hormone in females:
- Development of such a polyetiological syndrome as polycystic ovary syndrome;
- An ovarian tumor that, due to enlarged granulosa, increases AMH levels.
The main thing in identifying such indicators is to identify the pathogenetic cause of the increase in this hormone.
Main indications for its use:
- Long-term infertility that is not controlled by drug treatment;
- Women have a history of several attempts to carry out an in vitro fertilization protocol, which ended in failure;
- Infertility of unknown etiology;
- Increased levels of follicle-stimulating hormone;
- Suspicion of polycystic ovary syndrome;
- suspicion of an oncological process in the ovaries.
If you have at least one of the above symptoms, you must consult a doctor for this test and further treatment. You should not self-medicate or postpone diagnostic procedures for later. This leads to aggravation of the underlying pathological condition and reduces the chances of a successful pregnancy.
As a result, we can say that the level of anti-Mullerian hormone is of great importance in planning pregnancies in women suffering from such a diagnosis as infertility. The level of this hormone makes it possible to identify a possible cause of infertility, formulate a plan for carrying out an in vitro fertilization protocol, namely a method of stimulating ovulation, in order to perform it as carefully as possible with minimal complications and obtain the desired effect - the onset of such a desired pregnancy, which for some couples is the meaning of their whole life and will give you the happiness of being the best mom and dad for a new member of our society.
And under the federal program for carrying out the IVF protocol at the expense of the Mandatory Medical Insurance Fund, this dream becomes even closer to you. Having with you the results of examinations and a doctor’s opinion, for free IVF under compulsory medical insurance, you can submit an application on our website and finally find the happiness of motherhood and fatherhood.
Anti-Mullerian hormone (AMH) is called the egg counter. In men, it affects the formation of the genital organs and reaches a maximum during puberty. In women, it characterizes the quality and quantity of eggs. Its level decreases during menopause. Therefore, if AMH is low during reproductive age, a diagnosis of infertility is likely. Outwardly, this is not accompanied by any noticeable health problems. Medical examinations also show no pathologies. If conception does not occur for a long time, the doctor prescribes an extended “Efort test” to determine the level of a number of hormones, incl. anti-Mullerian.
Normally, AMH reaches its maximum in mid-maturity. Before and after this age its values are lower. Analysis of hormone levels is an achievement in recent years, because its amount in the blood is small. However, it indirectly characterizes the ovarian reserve.
What is ovarian reserve? This is the number of follicles in which eggs develop. It is formed in a girl at the embryonic stage and reaches a million pieces. But only a small part of the follicles goes through all stages of development and forms eggs capable of fertilization. Most of them die at different stages of development.
In a mature girl, the normal number of eggs reaches 300 thousand. If the ovarian reserve is reduced, then the likelihood of fertilization decreases. When AMH is higher or lower than normal, the ovarian reserve is proportionally altered. A more accurate determination of the ovarian reserve is possible using ultrasound, the criteria of which allow you to see and count follicles:
- the presence of 11-25 pieces is a good chance of getting pregnant within several years;
- less than 5 pieces - the chances are low, conception cannot be delayed;
- more than 30 pieces - may indicate polycystic disease.
An ultrasound examination allows you to track a woman’s monthly cycle and analyze whether the eggs are capable of fertilization.
Stages of research throughout the menstrual cycle.
- The first days after menstruation (no later than 10 days) – one or more dominant (15 mm) follicles are just beginning to grow.
- Every next two days, changes in dominants are monitored (follicles ready for ovulation reach 18-24 mm).
- The process of ovulation - if a stigma (protrusion) has formed in the wall of the follicle, the wall has torn and the egg has come out, ovulation has been successful.
- After ovulation, free fluid is observed outside the ovary and the corpus luteum inside it.
- In the absence of ovulation, the study is carried out before the start of the menstrual cycle. The dominant that has not reached ovulation forms a cystic follicle.
Low AMH levels and a regular lack of ovulation indicate that the eggs are defective and unable to reach maturity. If the situation does not change after hormonal therapy, a decision may be made to conduct IVF with donor embryos.
The essence of the anti-Mullerian hormone test and preparation for it
Analysis of the AMH level indicates the quantitative content of follicles in the 2nd stage of development (antral). The secondary follicle actively synthesizes hormones (estrogens, androgens, progestins). It becomes an element of the endocrine system. The normal level of the hormone in the blood is 1.1-2.4 ng/ml. If the test result is below 1.0 ng/ml, then the likelihood of pregnancy is minimal. Low AMH indicates the inability of the follicles to produce the necessary hormones that allow a woman to become pregnant, hence the diagnosis of infertility. A normal AMH level gives the patient a chance to become pregnant naturally.
The doctor who ordered a blood test for AMH to determine the chances of pregnancy will give recommendations on how to prepare for the test. Here are some rules.
- The best time for delivery is 3-5 days of menstruation, when the hormone level is stable.
- Avoid physical and emotional stress for three days before blood sampling.
- Do not drink alcohol 24 hours before the procedure, do not smoke for 3 hours.
- Take the test in the morning on an empty stomach, break from food for 8-12 hours (you can drink clean water).
- Fever, acute painful conditions are contraindications for testing.
You should not come to the treatment room after physiotherapy, massage, x-rays or fluorographic examination.
The main reasons for changes in AMH levels
At the onset of menopause, a decrease in AMH levels (to 0.05 g/ml after 50 years) is considered a natural process due to the fact that the ovarian follicular reserve is depleted. During reproductive age, this is an alarming symptom. It may indicate a developmental delay, hereditary pathology, the presence of a malignant tumor in the ovaries, or hormonal imbalances.
External manifestations of the problem are delay or absence of menstruation, scanty discharge during menstruation, problems with conception.
If an abnormal result is obtained, the analysis should be repeated, following all the rules for preparing for the analysis. It is advisable to check the result in different laboratories.
AMH above normal value
The most common cause of elevated AMH levels is polycystic ovary syndrome. In this case, the egg develops partially and cannot break through the follicle membrane. It freezes, forming a cyst. At the same time, the ovaries increase in size, which can cause pain in the peritoneum. Treatment with estrogens and antiandrogens, surgery and a combination of 2 methods is used.
Other reasons:
- genetic defects and mutations of the LH and AMH receptor;
- pathology of sexual development;
- granulosa cell tumor of the ovary;
- normogonadotropic anovulatory infertility (lack of ovulation due to trauma, abortion, sudden weight loss, infections, thyroid dysfunction, etc.).
In breastfeeding women, natural anovulatory infertility may temporarily occur.
AMH below normal value
More often than not, conception does not occur when decreased AMH. The main and natural reason is adulthood. If ovarian depletion has occurred, only IVF with donor embryos can save the situation.
Other causes of low AMH:
- small ovaries (less than 3 cm³);
- dysfunction of the pituitary gland, hypothalamus, thyroid gland;
- improper metabolism, fat metabolism;
- violation of the timing of puberty.
The situation is aggravated by smoking and sexually transmitted infections.
Treatment tactics for low AMH

Treatment for low AMH, according to many doctors, is impossible. Taking medications will not increase the number of follicles. But some of them stimulate the maturation of eggs in secondary follicles.
DHEA gel capsules of plant origin have good reviews. Puregon, Gonal, Menopur, Phostemon, 450 are also used according to special schemes.
There is a medical opinion that increased blood circulation in the pelvis promotes the development of eggs. To do this, they use warming up the ovaries, special massages, exercises, physiotherapy, running in combination with taking medications. There is a greater chance of getting pregnant with low AMH if FSH (follicle stimulating hormone) does not exceed the norm.
IVF with low levels of Anti-Mullerian hormone
Often, reproductive specialists do not accept patients for IVF with low AMH if the hormone level is less than 1.0 ng/ml and the age is close to 40 years. But if you talk to women who have become IVF mothers and read comments on the Internet, you can find many examples with AMH of 0.8-0.9 and even 0.7 ng/ml.
The last chance for low AMH, high FSH and late age is implantation of donor eggs. Many women do not accept this. Such a delicate issue, of course, is decided by the family.
IVF protocols for low AMH
AMH for IVF is crucial because... with indications less than 0.8-1.0 ng/ml, doctors rarely take patients for procedures, especially under free programs and quotas. During the examination, it is necessary to determine the level of FSH and the number of secondary follicles using ultrasound.
IVF protocols can be long or short.
- The long-term protocol begins a week before your period. Over the course of 21 days, the ovaries are stimulated with shock doses of hormones, a puncture with a large number of eggs (up to 20 pieces) is taken, and they are fertilized. Viable embryos are implanted into the mother's body at the age of 3 or 5 days. The danger of this option is possible hyperstimulation with severe complications.
- In the short version, the procedure begins on the 2-3rd day of menstruation, stimulating not the ovary, but the egg. Several dominant follicles are selected. With this method, there may not be enough quality eggs. The protocol is used for women with good ovaries.
The percentage of successful implantations is normally 20-60%, depending on age, egg quality, and the hormonal state of the female body. The technique is developing year by year, including due to an increase in the level of examination and diagnosis. Knowing the AMH level, the doctor more correctly chooses an infertility treatment strategy.
